HCV or Hepatitis C is the most common blood-borne infection in the world, with at least 3.8 million people living with it. Of this group, about 25% are co-infected with HIV and HCV. In recent years there’s been increased attention to HCV as new medications have been developed and cure rates have improved for nearly all people living with the disease. With the fast pace of drug development and the blur with which treatment guidelines change, it can be hard for medical providers and people living with HCV to keep up.
Utilizing information from current research and “Recommendations for the Testing, Managing and Treating of Hepatitis C,” put out by the American Association for the Study of Liver Diseases (AASLD) and Infectious Diseases Society of America (IDSA), this article will provide a basic overview of HCV testing, prevention, and treatment overall, with information that is specific for gay men.
Hepatitis C Testing
In reality, there is nothing specific or unique about HCV risk for gay men. That is to say, gay men aren’t at any greater risk for HCV than anyone else. With HCV, it’s the risk factors that matter: It’s the things we do regardless of sexual orientation or gender that determine if one should be tested for it.
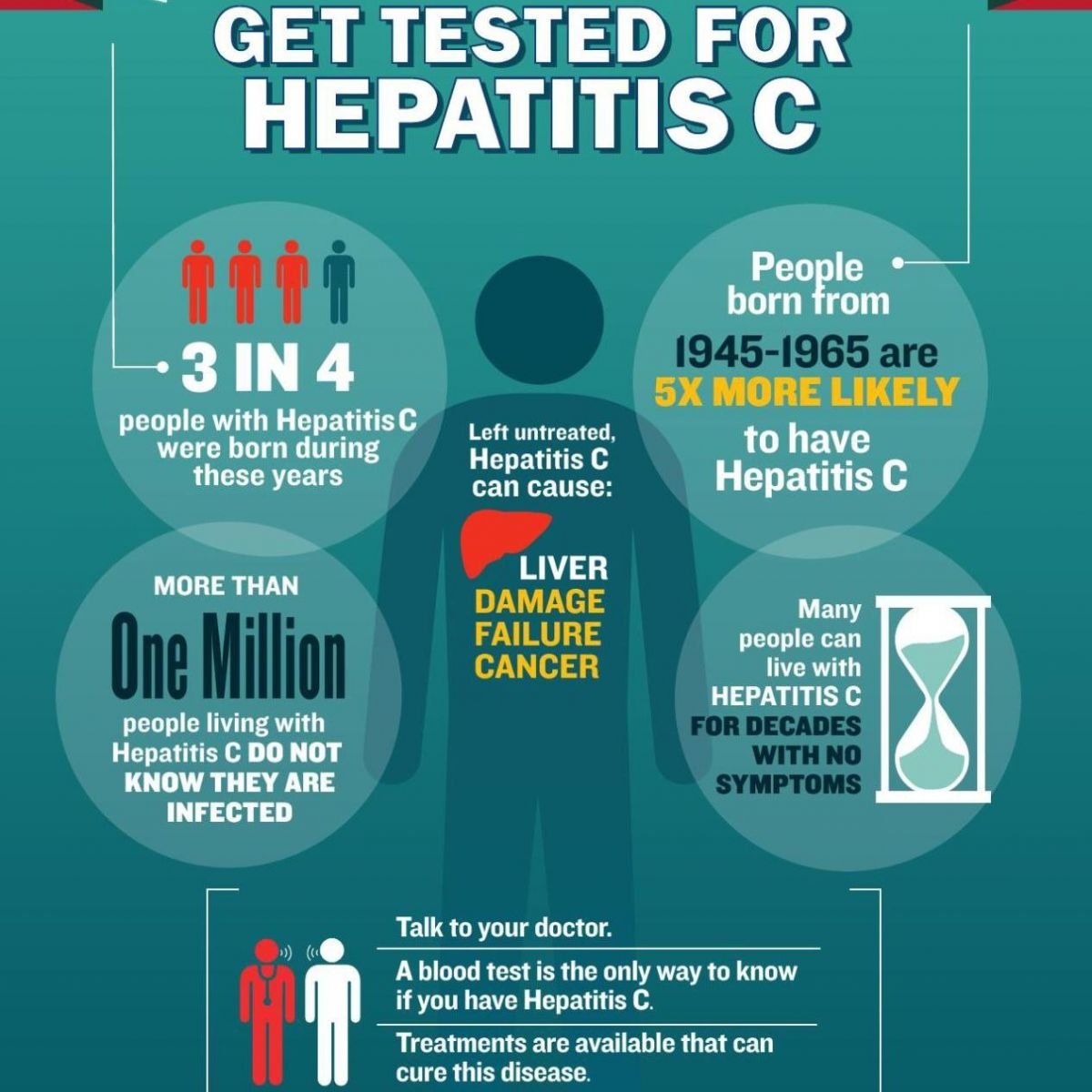
If you are at ongoing risk through injection drug use and/or are living with HIV and sexually active, you should test for HCV at least once per year.
Typically, Hepatitis C is not routinely screened for during annual physicals or other medical provider visits. In fact, while many people just assume that HCV gets screened during STD exams, it rarely does. If you think you need a test, you should ask for it. Your medical provider may ask you some questions and do a risk assessment so they can justify the ordering of the test and provide you with proper care and health education.
Testing for Hepatitis can be pretty complicated. It’s a two-step process: First, you take an HCV antibody test; and second, if the antibody test is positive, you take an HCV viral load test (also called HCV RNA or HCV PCR) to confirm that you are chronically infected with HCV.
The most important thing to remember here is this: If you test positive on the HCV antibody test, you have to confirm it with that viral load test.
If one has been told “you are positive for hepatitis C because you tested positive for the antibody test,” then you should follow up with the question “Are you sure? Did you confirm that antibody result with an HCV viral load?” If they didn’t do a viral load test, ask for one. Seriously: You’d be surprised how frequently this gets missed by medical providers.
Two Types Of Tests
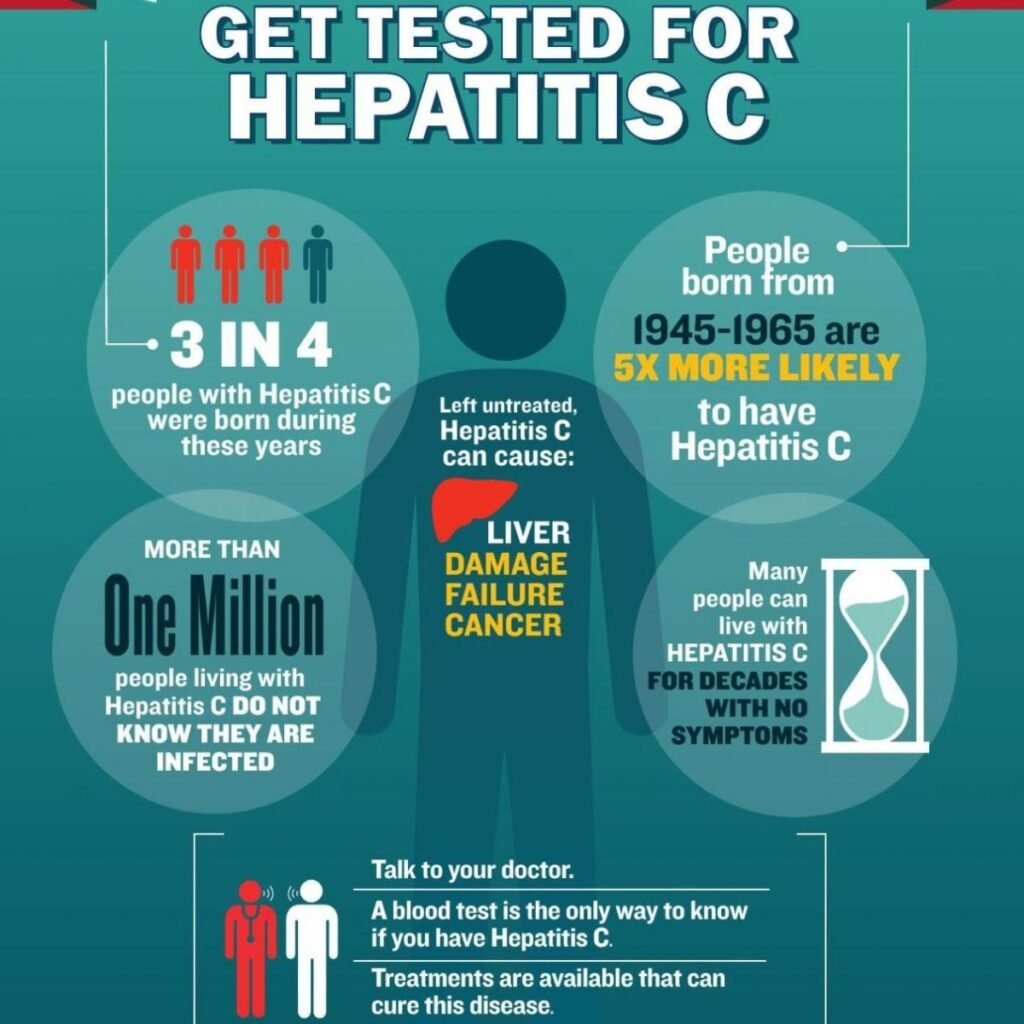
Similar to HIV, if you get infected with HCV, your body will respond by making antibodies (protein from your immune system). You’ll have these antibodies for the rest of your life. The thing that’s important to remember: Some people clear the virus within six months of infection, that is, there is no more virus in your body doing damage to your liver. This happens about 25% of the time (1 out of 4 people).
When you clear the virus, you will test positive for the antibodies, but not have the virus in you. Therefore, to know if you’re chronically infected or not, you need to confirm that positive antibody test with a viral load test.
Hepatitis C Prevention
HCV or Hepatitis C is mainly transmitted from blood to blood contact when someone shares a syringe or other injecting equipment with someone infected with the virus. The gold standard of HCV prevention is using a new syringe and unused injection equipment each and every time you inject, and you never have to share anything. This is easier said than done: Sometimes you have no other option but to re-use a syringe. When faced with this situation, there are things you can do to help prevent infection.
The primary way in which HCV infection occurs is through the sharing of syringes: That’s where the most blood is and that is the most direct way for HCV to get into a person. That said, the sharing of other injecting equipment cookers, cotton, water can lead to HCV infection, too.
The best way to prevent HCV infection while injecting drugs is to use a new syringe and unused injecting equipment each time you inject. If you have to re-use a syringe, try to mark it as your own so as to avoid accidentally using someone else’s syringe.
If sharing a syringe is the only option available, rinse the syringe with bleach to try to disinfect it and kill off any HCV that may be in there. (Remember to rinse it well afterwards.) A recent study has found that bleach was highly effective in killing HCV, but it’s important to note that it’s not a guarantee to prevent infection. From a harm reduction perspective, it’s better than nothing, but again, the gold standard for preventing HCV is to use a new syringe for each injection you do.
Hepatitis C Transmission Through Sex
HCV transmission through sex of is a complicated topic. HIV status appears to be the single greatest risk factor for gay men. Rates of HCV in HIV-negative gay men are much lower than in HIV-positive gay men. Research has shown that HIV-negative gay men are at low risk of HCV, and, as with non-injection drug using, HIV-negative heterosexuals, routine screening for HCV is not warranted. This research flies in the face of what many people assume: Gay men have anal sex and anal sex can lead to bleeding. Since blood can transmit HCV, many assume that anal sex will transmit the virus. While the data suggests little risk, the concerns and anxiety about the risk remain high.
Most of the time, HIV-positive gay men are at higher risk of sexually acquired HCV than are other groups. That said, it can still be a little complicated when you start to break it down. For example, we know that HCV is transmitted from blood-to-blood contact, but what about sexual fluids? There are some small studies that have found HCV in semen and non-bloody rectal fluids, while others have not. Whether it’s in semen or not, we know it’s in blood, and sexual practices that can lead to blood carry risk for HCV transmission.
In research studies that have looked at possible risk factors associated with sexual transmission of HCV, several behaviors have been identified: condomless anal sex, group sex, fisting, and so on. So, what accounts for the higher rates in this population? One possible explanation is sero-sorting, or the practice of only having sex with men who have the same positive HIV status. Many positive gay men have taken to this practice to prevent transmission to HIV-negative sex partners. Gay men may be aware of their partner’s HIV status, but not their HCV one, and if they practice condomless anal sex (or fisting) their risk for HCV is higher.
So what is the role of HIV itself and the risk of HCV acquisition from sex? It certainly makes sense that a weaker immune system can make one more vulnerable to HCV infection. Research is limited, but there may be a relationship between lower CD4 counts and increased risk of HCV acquisition. Additionally, rates of HCV were higher in HIV-positive gay men with lower CD4 counts even when they had fewer risk factors for HCV. We do not yet know what the protective factor of taking anti-HIV medications might provide against sexual transmission of HCV, but we do know all of the health benefits it provides otherwise. Regardless of CD4 count, you want to minimize your risk of blood contact to minimize the risk of HCV transmission. The following section reviews the risk factors for sexual transmission of HCV that have been identified in a variety of studies looking at HIV-positive gay men.
Hepatitis C Re-Infection
One can get hepatitis C more than once. This is weird and can be a little confusing, and there is a lot of misinformation out there among both patients and medical providers about this.
Like many viruses (like the herpes virus that causes chicken pox) or even other types of hepatitis viruses (like hep A and hep B), you can get it and your body makes antibodies and immunity to fight off any future infection. In other words, if you get it once, you’re not going to get it again.
When one get infected with HCV, one’s body produces antibodies in an effort to fight the infection. As stated above, it’s the antibody test that used to detect a possible infection. If this test is positive, then we follow it up with a viral load test to look for the actual virus.
About 1 in 4 (25%) people clear HCV in the first six months of infection on their own. A person who clears it will always have HCV antibodies but no more virus to do any damage to their liver. These antibodies don’t protect them from a future infection, and they can still get re-infected and get HCV again. Again, the person can get HCV and clear the virus again (or even multiple times), but there’s always a risk that the next time will lead to chronic infection.
HCV re-infection occurs when a person has detectable HCV virus in their blood after he or she has either been cured through treatment or after they have spontaneously cleared the virus on their own.
If one is among those 25% of people who cleared it naturally, or you were treated and cured, you’re going to have HCV antibodies. You’ll still want to do all you can to stay HCV negative and avoid re-infection. Additionally, if you’re one of these people and you have ongoing risk for re-infection, you want to test regularly at least annually by doing a HCV viral load test as the antibody test won’t tell you anything about a new infection.
Hepatitis C Treatment
If one was to talk to someone who was treated for HCV as little five years ago, you would likely hear horror stories of a year of treatment, complete with weekly injections of a medication that would make a person feel as though they had the worst flu of their life. For all of the misery, only about 50% of people would be cured. The treatments were so bad and the options so poor that many people chose not to test at all as they didn’t want to know if they had it since they would never take (or, in the case of some medical providers, would never prescribe) the medications available.
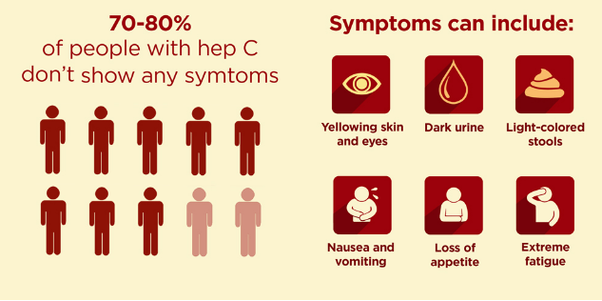
Currently, hepatitis C can be cured in just about everybody with 12 (in some cases 24) weeks of pills (no injections!) and very tolerable side effects. With the effectiveness and relative ease of treating and curing all people with HCV, the AASLD/IDSA HCV Guidance Panel recommends HCV treatment for all people living with the virus, except in the few circumstances where a person has a very low life expectancy where said treatment won’t make a difference.
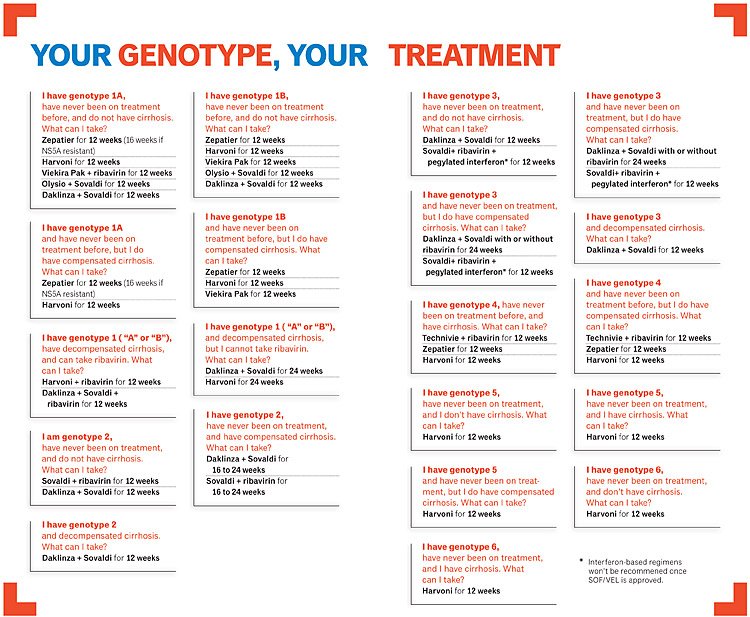
We can even treat people with very advanced liver disease cirrhosis and we can treat people who are both on the liver transplant list or who have received a liver transplant. It’s complicated, but with a liver specialist to manage care and treatment, successful cures are possible for even the most advanced of cases.
Hepatitis C Treatment In Hiv/Hcv Co-Infected Persons
HCV/HIV co-infection is a serious medical issue. As discussed above, there is increased risk of sexual transmission of HCV in this population, but HIV also appears to speed up HCV-related liver disease. For these reasons and more, the AASLD/IDSA HCV Treatment Guidance recommends treatment for all HIV/HCV co-infected persons, just as they recommend it for all HCV-mono-infected persons. Similarly, all co-infected persons can be treated with almost all of the available regimens that a person without HIV can take. It can get complicated, and you want to make sure that your HIV provider and HCV provider (if they are not one and the same) are in regular communication with one another and each knows what the other is prescribing to avoid any drug-drug interactions.
Parting Words
Fortunately, we are in a remarkable time for the care and treatment of hepatitis C. In theory, we can treat and cure everyone and eradicate the virus from the planet. We have a long way to go, but increasing education and awareness, testing for the virus as needed, preventing primary infection and re-infection, and engaging in medical care will get us there.
Gay Health News recommeneds that the key strategies for all gay men to adopt are early and frequent screenings, early treatments and always to be careful and adopt preventive measures.